
EFFECTIVE CONTRACEPTION THAT ALSO HELPS WITH HEAVY PERIODS1
WHAT IS MIRENA®?
Mirena® is a small device called an intrauterine system (IUS) that is placed in your uterus (womb) by a specially trained healthcare professional - usually a doctor or a nurse - to prevent pregnancy for up to 8 years. Mirena® is effective for 5 years for heavy menstrual bleeding (idiopathic menorrhagia) ). Mirena® should be removed or replaced when the heavy menstrual bleeding or painful menses return or after 8 years at the latest.
Mirena® is effective for protection from excessive growth of the lining of the womb (endometrial hyperplasia) during estrogen replacement therapy for 5 years. If you are using Mirena® for this reason, your Mirena® should be removed after 5 years.1
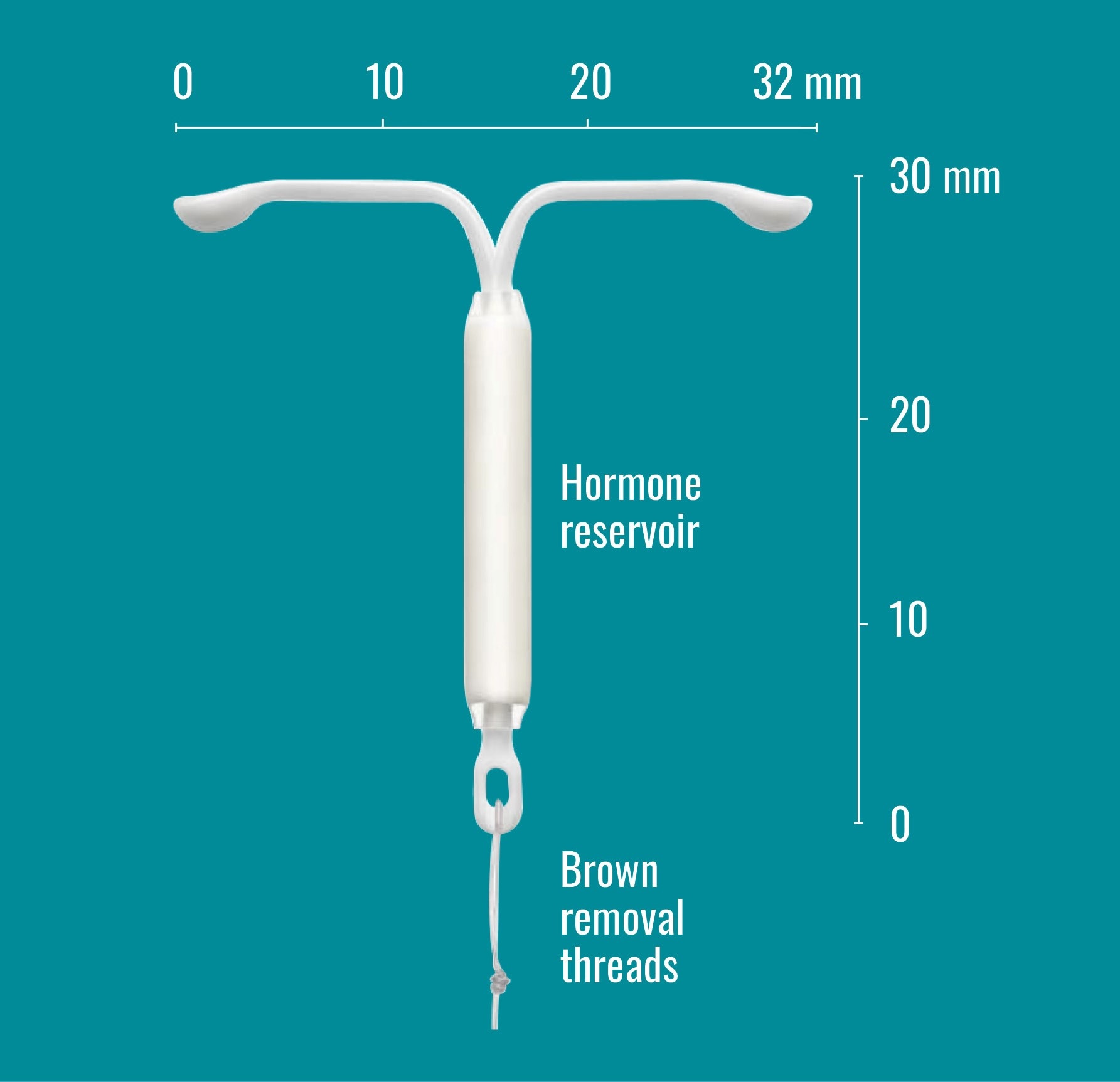
- Small and T-shaped
- Made of soft, flexible plastic
- Contains a tiny cylinder with a small amount of the hormone levonorgestrel
- Two fine threads attached to the base of the frame to help with removal by a healthcare professional and to help to check that Mirena® is still in place
KEY FEATURES OF MIRENA®
- It is over 99% effective at preventing pregnancy1
- It is registered for up to 8 years of continuous use but can be removed by a healthcare professional at any time if you wish to stop using Mirena® for any reason1
- It does not require daily pill taking or regular injections1
- It is quickly reversible and does not impact your chance of having a baby in future1
- It may reduce your period pain1
- While many women experience frequent spotting or light bleeding in addition to their periods for the first 3–6 months, over time you are likely to have a gradual reduction in the number of bleeding days and in the amount of blood loss each month. You may even find that your periods stop altogether1
- It is the most effective medical treatment available for heavy menstrual bleeding (heavy periods) when there is no underlying medical condition causing the heavy periods.2 It can be used for heavy menstrual bleeding for up to 5 years, or when painful menses return or after 8 years at the latest.1
For information about Mirena® to treat heavy menstrual bleeding click here
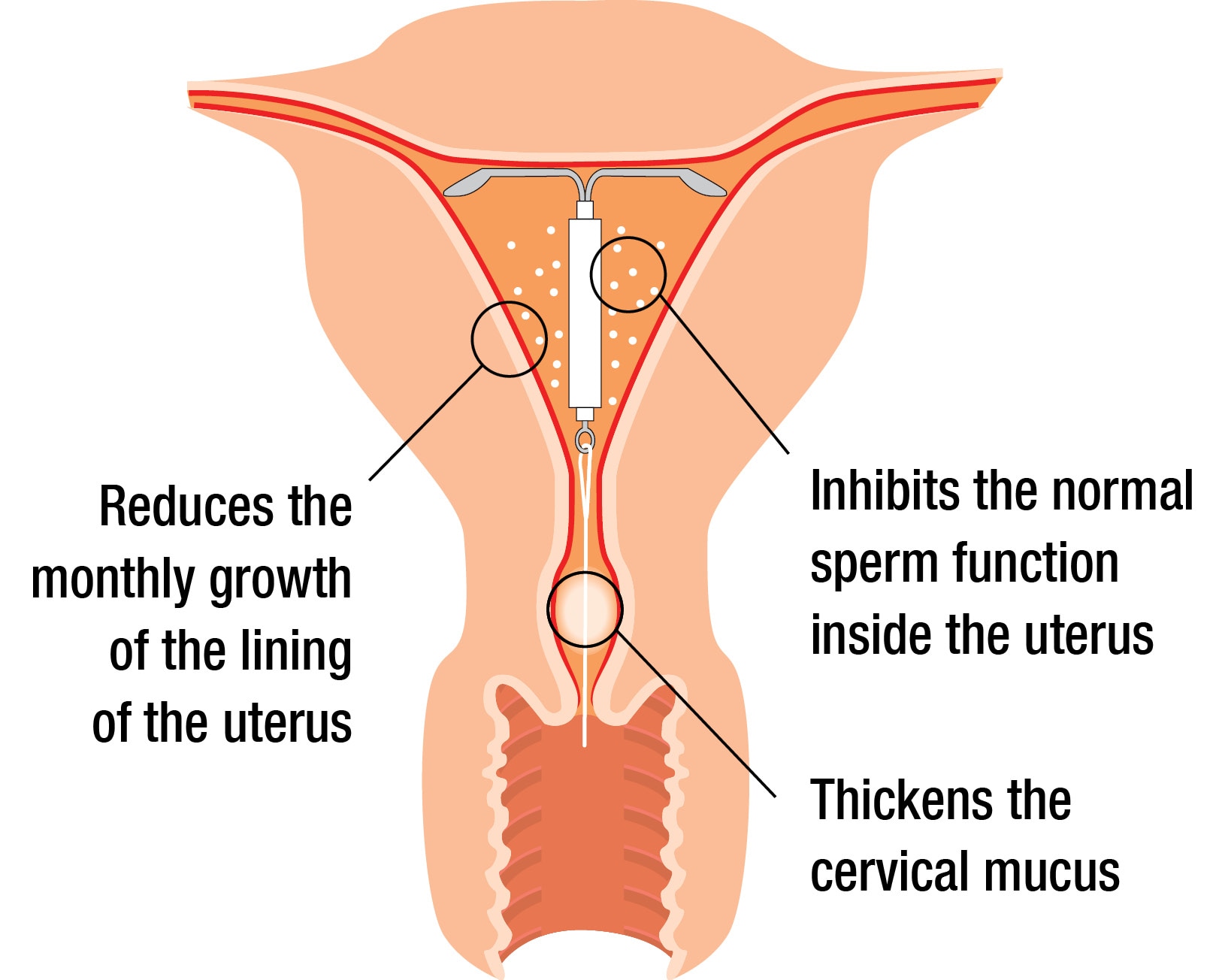
HOW DOES MIRENA® PREVENT PREGNANCY?
Mirena® contains a hormone called levonorgestrel, which is similar to the progesterone hormone made by your body.
This hormone prevents pregnancy by:1
- Thickening the mucus in the cervix making it harder for sperm to reach the egg
- Stopping sperm moving normally inside the uterus, preventing fertilisation
- Controlling the monthly growth of the lining of the uterus so that it is not thick enough for you to become pregnant
WHERE CAN I GET MIRENA®?
Mirena® is a prescription medicine, and it must be inserted by a specially trained healthcare professional (e.g. doctor or nurse).
There are a number of different types of healthcare providers that may offer Mirena® including:
- Some specially trained GPs and nurses
- Sexual Wellbeing Aotearoa clinics
- Sexual health clinics
- Surgical abortion providers
- Specialist gynaecology clinics
DEPENDING ON THE PROVIDER, YOU MAY NEED TO ARRANGE TWO VISITS:
VISIT 1: To discuss your contraceptive options and make sure that Mirena® is right for you and to have any health checks that the provider decides are necessary.
VISIT 2: To have the Mirena® inserted.
If you’re not sure who to speak to first and you don’t have a usual doctor, you may wish to contact Sexual Wellbeing Aotearoa. Sexual Wellbeing Aotearoa website www.sexualwellbeing.org.nz has a clinic finder so you can find a clinic near you, along with clinic contact details. Appointments are free for women under the age of 22.
HOW MUCH WILL IT COST?
Mirena® device
Mirena® is a fully funded medicine, which means you should just have to pay the normal pharmacy dispensing fee for the Mirena® device itself. If you don’t normally pay for your prescriptions, then the Mirena® may be free. If you are not sure, check with your pharmacist.
Mirena® insertion
The cost to have Mirena® inserted can depend on a number of different factors including:
- The health provider that is inserting your Mirena® (e.g. hospital, GP clinic, private gynaecologist, Sexual Wellbeing Aotearoa clinic)
- The reason you are having Mirena® (in some cases private health insurers or your local health authority may fund Mirena® insertion if it is to treat a health condition)
- Your personal circumstances (e.g. your age, whether there is special funding available in your local area)
Talk to your healthcare professional or contact Sexual Wellbeing Aotearoa clinic for more information about the cost of having Mirena® inserted.
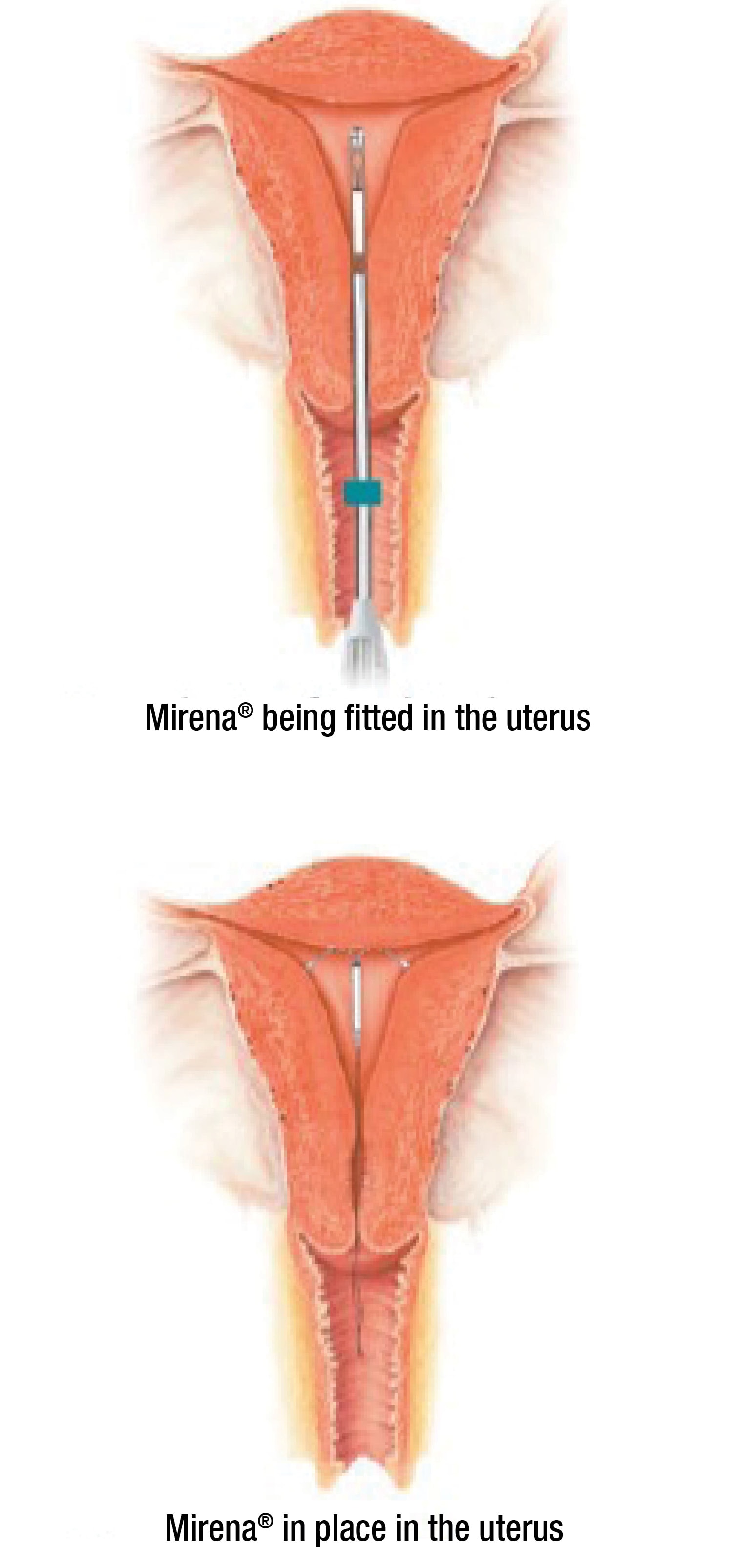
THE PLACEMENT PROCEDURE
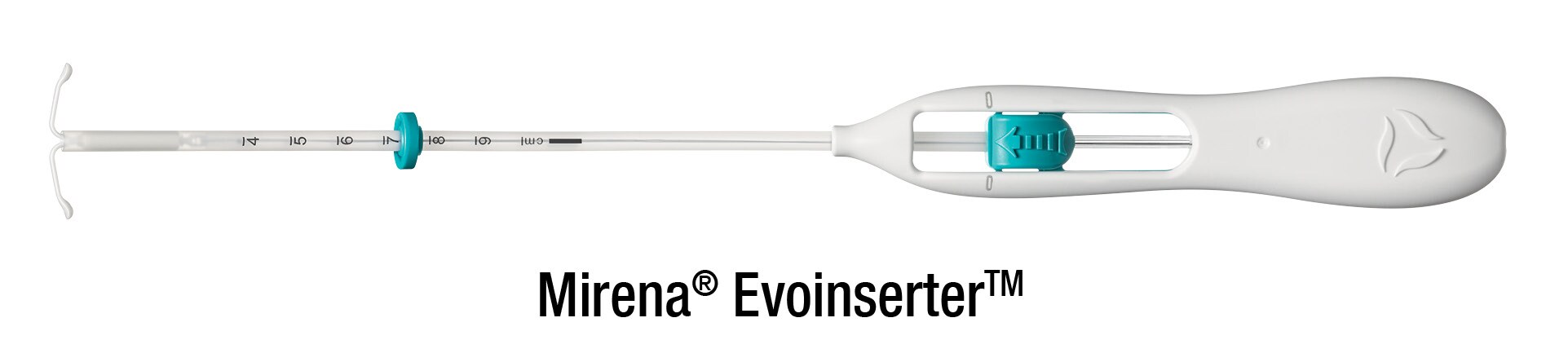
Mirena® is a small T-shaped device about 3 cm long. When you collect Mirena® from the pharmacy, you’ll notice it is supplied in a long thin box as the device comes with its own special insertion tube, used to place Mirena® into your uterus.
Talk to your healthcare professional about when to have Mirena® inserted. For most women who don’t already have a Mirena® (or Jaydess®) in place, the best time is within 7 days of the start of your period. Depending on your situation, your healthcare professional may need to check you are not pregnant before inserting Mirena®.1
THE INSERTION PROCESS
- To help place Mirena® in the correct position, your healthcare professional inserting Mirena® will perform an examination to determine the size and position of your uterus.
- The plastic tube containing Mirena® is inserted through your vagina into the uterus. Some discomfort or cramping is common at this time.
- Once Mirena® is in the correct position, the plastic insertion tube is withdrawn, leaving Mirena® in your uterus. The threads of Mirena® are then trimmed. The threads are there so it can be checked whether Mirena® is still in place and to help with removal of Mirena® (by a healthcare professional) when required.
Everyone’s experience of Mirena® placement is different and while it can be uncomfortable, many women feel only mild pain or no pain at all.3 Talk to your healthcare professional about what to expect during and after insertion of Mirena® and if you are concerned about the possibility of pain ask about potential options for pain relief before the procedure.
If you experience excessive pain or bleeding during or after insertion of Mirena®, or if you continue to feel pain, tell your healthcare professional immediately.
For more information about what to expect during and after insertion of Mirena® download a copy of the patient information booklet.
SAFETY INFORMATION
WHAT ARE THE MOST COMMON SIDE EFFECTS FROM USING MIRENA®?
All medicines can have side effects. Some women may experience side effects while using Mirena®, while others may not experience any. Side effects are most common during the first months after Mirena® is inserted and decrease as time goes on.
Period bleeding pattern changes1,4
It is very common for periods to change after having Mirena® inserted. In the first few months of use the bleeding pattern may include spotting, shorter or longer periods, or irregular bleeding. After an initial increase in the number of bleeding or spotting days per month this should decrease over time. Some women eventually stop bleeding each month because Mirena® can be so effective at stopping the monthly growth of the lining of the uterus.
If you have been using Mirena® and are having it removed and replaced at the same visit, the initial increase in bleeding you may have experienced with your first Mirena® is unlikely to recur.
When Mirena® is removed, periods can be expected to return to their previous pattern, unless menopause has been reached.
Other very common events1
The following is a list of other events reported by at least 1 in 10 women during clinical trials of Mirena®.
If you are concerned about the possibility of side effects speak to your healthcare professional for advice.
- Lower abdominal/pelvic pain
- Headache
- Vulvovaginitis (inflammation or infection of the vulva/vagina)
- Vaginal discharge
Tell your doctor or pharmacist if you notice any side effects following insertion of Mirena®, particularly if they worry you.
More information
For information about other possible side effects – including rare but serious complications – and other important things to be aware of when using Mirena® speak to your healthcare professional and review the following resources:
References: 1. Mirena® Data Sheet, 10 April 2025. 2. Heavy Menstrual Bleeding Clinical Care Standard. Australian Commission on Safety and Quality in Health Care. https://www.safetyandquality.gov.au/standards/clinical-care-standards/heavy-menstrual-bleeding-clinical-care-standard; accessed June 2025. 3. Gemzell-Danielsson K, et al. Fertil Steril. 2012;97:616-622. 4. Mirena® Consumer Medicine Information, April 2025.
MIRENA® (levonorgestrel). MIRENA® is an intrauterine system containing 52 mg levonorgestrel, which is slowly released at an initial rate of 20 mcg/24 hours. MIRENA is a Prescription Medicine for contraception and is effective for 8 years for prevention of pregnancy . MIRENA is also a treatment for unexplained heavy menstrual bleeding where no underlying pathology causing excessive bleeding can be found. Mirena is effective for 5 years for heavy menstrual bleeding. MIRENA is effective for 5 years for protection of the lining of the womb when oestrogen therapy is prescribed for menopausal symptoms. MIRENA must not be used during pregnancy, if there is any sign of pelvic or genital tract infection, inflammation or cancer, if there is womb or cervical abnormality, confirmed or suspected hormone-sensitive cancer including breast cancer, undiagnosed abnormal bleeding, active liver disease or if you are allergic to any ingredients in MIRENA. MIRENA should be inserted by a doctor who has been trained in the insertion technique. Removal of MIRENA is recommended if the following medical conditions occur: an increased susceptibility to infections, acute infection not responding to treatment. Migraine or severe headaches, jaundice, increased blood pressure, hormone-sensitive cancer, stroke, severe heart or blood vessel disease, blood clots may occur during MIRENA use, should this happen; your doctor may consider removal of MIRENA. MIRENA should be used with caution if you have diabetes or a heart condition from birth and are at risk of infection. MIRENA must be removed if pregnancy (which might be outside the womb) or puncture of the womb is suspected or if MIRENA is partially expelled. MIRENA does not protect against HIV infections (AIDS) and other sexually transmitted infections. The pattern of side effects, which are more common in the first months of use, should be explained to you. Commonly reported side effects include changes to menstrual patterns, painful menstruation, genital discharge, redness, or itching, headache/migraine, abdominal, breast or back pain, depressed mood, nervousness, nausea, acne, weight changes, decreased libido, excessive hair growth, benign ovarian cysts and expelled device. The possibility of side effects such as puncture of the womb, allergic reactions, bacterial infection of the blood, breast cancer, or pregnancy outside the womb should be discussed with your doctor, pharmacist or health professional. If symptoms persist or you have side effects, see your doctor for advice. MIRENA is a fully funded medicine – a pharmacy charge and normal Doctor’s visit fees and insertion fees may apply. MIRENA has both risks and benefits. Use only as directed. Consult your doctor to see if MIRENA is right for you. For more information, read the Consumer Medicine Information available at https://www.medsafe.govt.nz/Consumers/cmi/m/Mirena.pdf Bayer New Zealand Limited, PO Box 2825, Shortland Street, Auckland 1140, telephone 0800 229 376.
Mirena® is a registered trademark of the Bayer Group, Germany.
PP-PF-WHC-NZ-0034-2. TAPS: NP23064 JULY 2025
